Bariatric surgery, while a beacon of hope for many struggling with obesity, harbors potential pitfalls that extend far beyond the operating room.
Story Snapshot
- Bariatric surgery is becoming more common, but risks remain significant.
- Immediate complications include bleeding and leaks; long-term issues involve nutritional deficiencies and hernias.
- Careful patient selection and multidisciplinary follow-up are crucial for minimizing risks.
- Differences in complication risks across surgical techniques necessitate tailored approaches.
Understanding Bariatric Surgery Risks
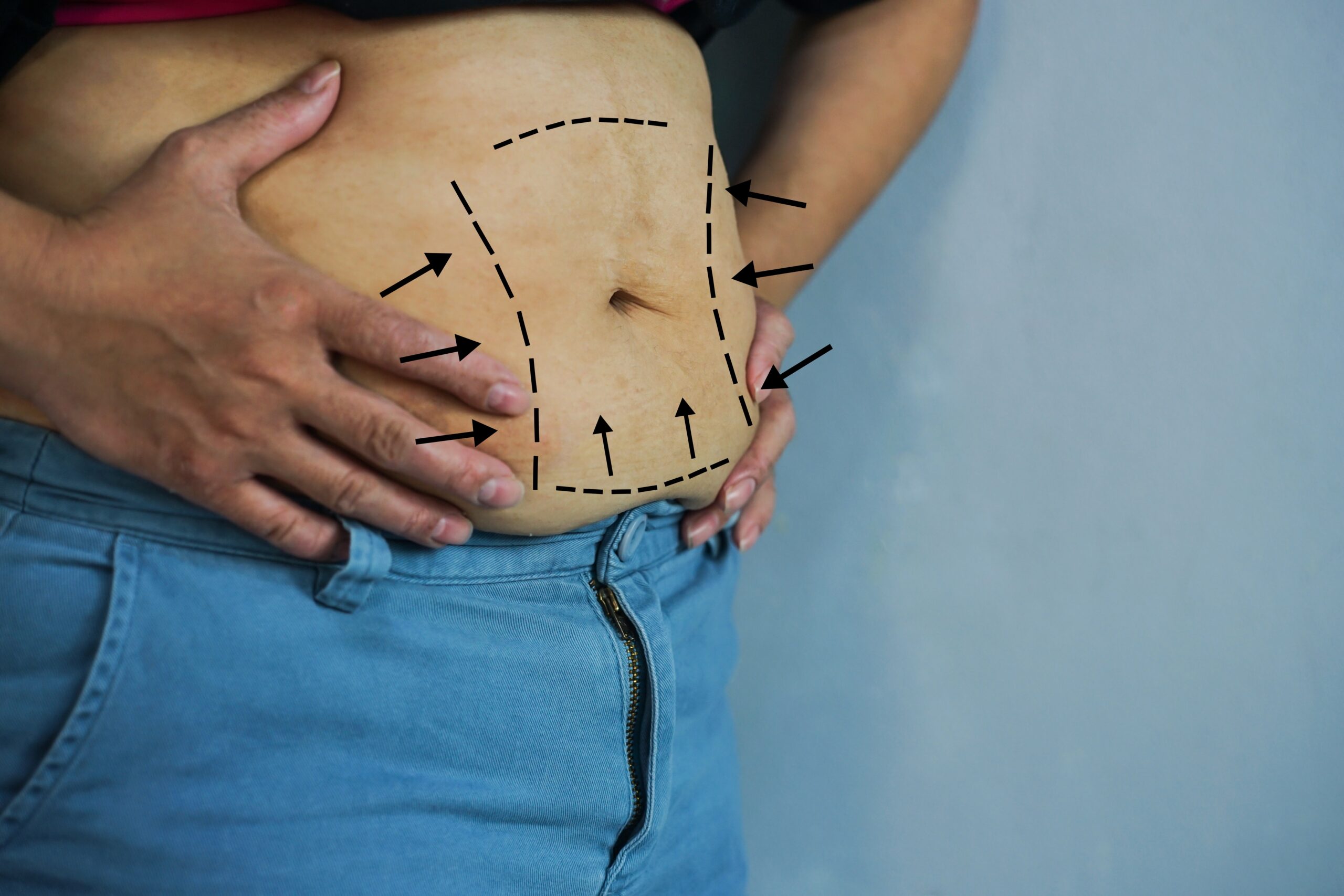
Bariatric surgery offers a life-changing solution for those battling severe obesity, yet it is not without its dangers. Immediate postoperative risks like bleeding and anastomotic leaks demand prompt attention. These complications, while statistically low, can have severe health implications. Long-term, patients may face nutritional deficiencies, internal hernias, and dumping syndrome. Such risks necessitate informed patient decisions guided by comprehensive risk disclosure and careful surgical planning.
Patients with severe obesity often have underlying health issues that heighten surgical risks. Conditions like diabetes and cardiovascular disease complicate recovery, increasing susceptibility to infections and delayed healing. The intricate balance of managing these comorbidities alongside surgical intervention requires a multidisciplinary approach, ensuring patients receive preoperative optimization and postoperative care that mitigate these inherent risks.
Chat safely, anytime, with My Healthy Doc.
Assessing Complication Rates and Mortality
Complication rates in bariatric surgery range broadly, with overall rates between 10% and 17%. Mortality rates, while low, vary by procedure type. Gastric bypass and sleeve gastrectomy have a 0.5% mortality rate, while malabsorptive operations are higher at 1%. Each surgical technique carries unique risks, and selection should be tailored to the patient’s individual health profile, prioritizing procedures that minimize specific risks while maximizing potential benefits.
Some complications require reoperation, with about 7% of patients needing additional surgical intervention. Conditions like internal hernias or anastomotic strictures may necessitate further procedures, underlining the importance of diligent postoperative monitoring. Patients who experience significant weight regain or fail to achieve desired weight loss might also require revisional surgery, highlighting the complex interplay of surgical choice and long-term patient outcomes.
Watch:
https://www.youtube.com/watch?v=Rtt6QkvLekg&vl=en
Got a health question? Ask our AI doctor instantly, it’s free.
Short- and Long-Term Impacts
In the immediate postoperative period, morbidity and mortality are significant concerns. Complications such as anastomotic leaks can lead to severe infections and organ failure if not swiftly addressed. Long-term, patients may suffer from nutritional deficiencies affecting quality of life. Thiamine deficiency, in particular, poses a risk for neurological complications, underscoring the need for ongoing nutritional monitoring and supplementation.
Patients may also experience gastrointestinal dysfunction, including dumping syndrome and bowel obstruction, which can severely impact dietary intake. Understanding these potential outcomes is crucial for both patients and healthcare providers to manage expectations and prepare for possible interventions.
Bariatric Weight-Loss Surgery and Mortality https://t.co/OmWtOmH8Y2
— Jane Harris (@janeharrisp_) December 30, 2025
The Role of Multidisciplinary Care
Successful bariatric surgery outcomes rely heavily on a coordinated, multidisciplinary care approach. Surgeons, nutritionists, and specialists must work together to address the wide range of complications that can arise both immediately and long after surgery. This collaborative care model is essential for optimizing patient outcomes, preventing complications, and managing any that do occur.
Given the complexities of bariatric surgery, comprehensive preoperative assessments and individualized postoperative plans are critical. Patients require lifelong follow-up to monitor for nutritional deficiencies and other complications. This long-term care commitment ensures that the benefits of bariatric surgery are fully realized while minimizing the risks that accompany such a transformative procedure.
Your new health companion is online, ready when you are.
Sources:
NCBI/NIH StatPearls
Circulation Journal
UPMC Clinical Guidelines
PMC/NIH Research
JAMA Surgery
NHS Clinical Guidelines